Hysteroscopy
A hysteroscopy
What is a hysteroscopy?
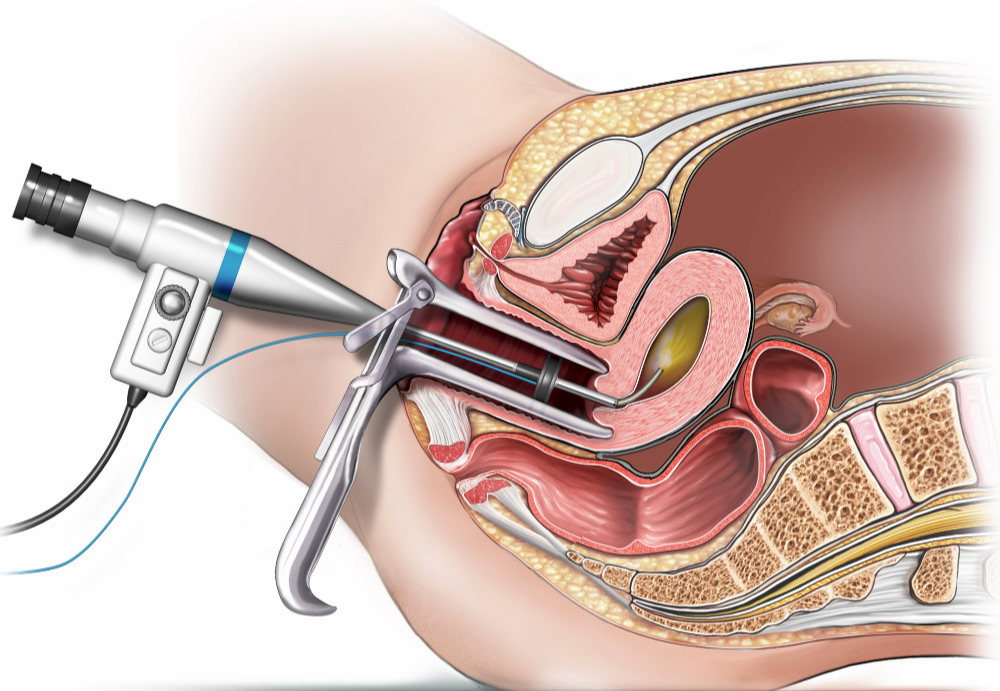
A hysteroscopy is a procedure to look at the inside of your uterus (womb) using a small telescope (hysteroscope). It is common for your gynaecologist to perform a biopsy (removing small pieces of tissue from the lining of your womb) at the same time.
A hysteroscopy is good for finding out the cause of abnormal bleeding from your womb, especially heavy periods and bleeding after menopause. It will help to find out if you have fibroids, polyps, endometrial cancer or an abnormally-shaped womb.
Are there any alternatives to a hysteroscopy?
An ultrasound scan and a biopsy using a small tube placed through your cervix (neck of your womb) may find the cause of your symptoms.
Your gynaecologist may recommend a specialised ultrasound (also called sono-hysterogram). This is where an ultrasound probe is placed in your vagina after your womb is filled with a saline (salt water) solution.
What will happen if I decide not to have the operation or the operation is delayed?
Your gynaecologist may recommend a scan and biopsy to find out more information but this may not accurately find the cause of your symptoms. Choosing not to have the procedure may make it more difficult for your gynaecologist to recommend the best treatment for you.
If you experience any of the following symptoms, contact your healthcare team:
- changes to your monthly bleeding pattern if you have periods
- increased abdominal (tummy) swelling
- worsening pain that needs more medication than you are currently taking.
What does the procedure involve?
The procedure can be performed under local or general anaesthetic, or without any anaesthetic, and usually takes less than ten minutes. You gynaecologist may examine your vagina. They will pass the hysteroscope through your vagina, through your cervix and into your womb.
Your gynaecologist will inflate your womb using gas (carbon dioxide) or a salt water fluid (saline), so they can have a clear view. They can use instruments to perform a biopsy or remove polyps and small fibroids. If your gynaecologist does this, the procedure will take a little longer.
What complications can happen?
Some complications can be serious an can even cause death.
Hysteroscopy complications:
- pain
- feeling or being sick
- bleeding
- infection
- allergic reaction to the equipment, materials or medication
- venous thromboembolism
- a small hole in your womb or cervix made by one of the instruments, with possible damage to a nearby structure
- failed procedure.
How soon will I recover?
The healthcare team will tell you what was found during the hysteroscopy and will discuss with you any treatment or follow-up you need. You should be able to go home the same day.
You should be able to return to normal activities the next day. You may get some cramps and mild bleeding similar to a period.
Regular exercise should improve your long-term health. Before you start exercising, ask the healthcare team or your GP for advice.
Summary
A hysteroscopy is usually a safe and effective way of finding out if there is a problem with your womb and, for some women, treating your symptoms.
Where to get help
Last reviewed: 07-07-2023
Acknowledgements
Patient Safety & Clinical Quality
EIDO Healthcare Australia

The operation and treatment information on this page is published under license by Department of Health Western Australia from EIDO Healthcare Australia and is protected by copyright laws. Other than for your personal, non-commercial use, you may not copy, print out, download or otherwise reproduce any of the information. The information should not replace advice that your relevant health professional would give you.